What is Pseudomonas Aeruginosa, the bacteria responsible for the eyedrops infections
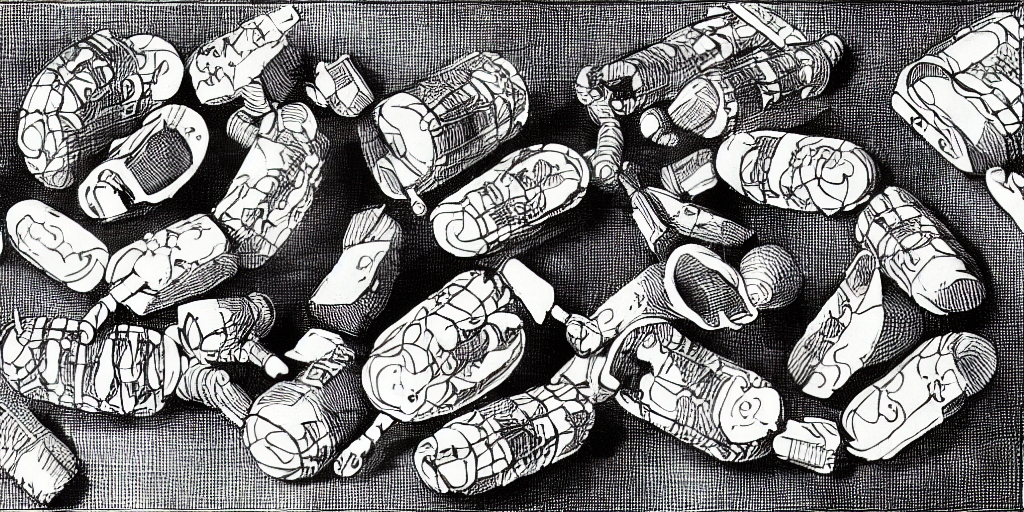
Pseudomonas aeruginosa is a Gram-negative, rod-shaped, and opportunistic pathogen that is commonly found in soil, water, and various moist environments. It has emerged as a significant cause of nosocomial infections, particularly in immunocompromised individuals and those with underlying medical conditions. Due to its intrinsic resistance to many antibiotics and its ability to form biofilms, P. aeruginosa poses a considerable challenge in clinical settings.
Pseudomonas aeruginosa was first identified by Carle Gessard, a French pharmacist, in 1882. Gessard initially named the bacterium "Bacillus pyocyaneus" because of its ability to produce a blue-green pigment called pyocyanin. The name was later changed to Pseudomonas aeruginosa, with "Pseudomonas" referring to the Greek words for "false" and "unit" and "aeruginosa" meaning "copper rust," describing the blue-green color of the colonies on agar plates.
Pseudomonas aeruginosa has been involved in several outbreaks and incidents, particularly in healthcare settings. Here are some notable examples:
- 2022-2023 - US Eyedrops Infections: An outbreak of eyedrops traced to production facility in India linked to dozens of infections, as well as cases of vision loss, surgical removal of eyes and deaths from the infections. Available at apnews.com
- 2017 - German NICU outbreak: P. aeruginosa was implicated in an outbreak in a neonatal intensive care unit, resulting in the deaths of three infants and leading to the temporary closure of the unit. Available at journal.lww.com
- 2016 - Italian hospital water supply outbreak: A P. aeruginosa outbreak in a hospital in Italy was traced back to a contaminated water supply, causing 17 confirmed cases and five deaths. Available at biomedcentral.com
- 2013 - UK hospital mouthwash outbreak: An outbreak in a hospital in the United Kingdom was associated with a contaminated alcohol-free mouthwash, leading to 11 confirmed cases and one death. Available at journalofhospitalinfections.com
- 2012 - Netherlands duodenoscope outbreak: A P. aeruginosa outbreak at a hospital in the Netherlands was linked to a contaminated duodenoscope used for endoscopic retrograde cholangiopancreatography (ERCP) procedures, resulting in 11 infections and two deaths. Available at cdc.gov
Biology and Ecology of Pseudomonas aeruginosa
P. aeruginosa is a metabolically versatile bacterium capable of surviving in diverse environments. It is an aerobic organism but can also grow under anaerobic conditions through denitrification. Its ability to produce a wide range of extracellular enzymes and metabolites allows it to utilize a variety of organic compounds as energy sources. The bacterium's adaptability and resilience are facilitated by its large genome, which encodes a wide array of regulatory and metabolic functions.
P. aeruginosa possesses several surface structures, including flagella, pili, and lipopolysaccharides (LPS), which are essential for its motility, adhesion, and immune evasion. The bacterium's ability to form biofilms further contributes to its survival and persistence in different environments, including medical equipment and indwelling devices.
Pathogenicity and Virulence Factors
P. aeruginosa can cause various infections, such as urinary tract infections, respiratory infections, skin and soft tissue infections, and bacteremia. The severity of the infection depends on the host's immune status and the bacterium's virulence factors, which include:
- Toxins: P. aeruginosa produces a range of exotoxins, including Exotoxin A, Exoenzyme S, and Exoenzyme U, which can disrupt cellular functions and induce host cell death. Additionally, it produces proteases and elastases that degrade host tissue and facilitate bacterial invasion.
- Quorum sensing: This is a cell-to-cell communication mechanism that allows P. aeruginosa to coordinate gene expression in response to population density. Quorum sensing regulates the production of virulence factors, including biofilm formation, swarming motility, and toxin production.
- Biofilm formation: P. aeruginosa can form complex, multicellular communities known as biofilms, which provide protection against antibiotics, host immune responses, and environmental stresses. Biofilms also contribute to the persistence of chronic infections, such as those associated with cystic fibrosis and chronic wounds.
Treatment and Antibiotic Resistance
P. aeruginosa's intrinsic resistance to many antibiotics and its ability to acquire resistance through mutation or horizontal gene transfer make it challenging to treat. Commonly used antibiotics include aminoglycosides, fluoroquinolones, and beta-lactams, such as piperacillin-tazobactam and ceftazidime. However, the emergence of multidrug-resistant strains has limited the effectiveness of these treatments.
Combination therapy is often employed to increase the likelihood of successful treatment and minimize the development of resistance. In recent years, alternative therapies have been explored to address the challenge of antibiotic resistance in P. aeruginosa infections. These include:
- Antimicrobial peptides: These are small, naturally occurring proteins that exhibit broad-spectrum antimicrobial activity. They can disrupt bacterial membranes, inhibit biofilm formation, and modulate host immune responses. Research is ongoing to develop synthetic antimicrobial peptides as potential therapeutics against P. aeruginosa.
- Bacteriophage therapy: Bacteriophages are viruses that specifically infect and kill bacteria. Phage therapy has been revisited as an alternative treatment for multidrug-resistant P. aeruginosa infections. The use of bacteriophages in combination with antibiotics has shown promise in preclinical studies and early-phase clinical trials.
- Immunotherapy: This approach aims to harness the host's immune system to combat P. aeruginosa infections. Strategies include the development of vaccines targeting specific virulence factors or surface antigens, as well as the use of monoclonal antibodies to neutralize bacterial toxins or promote opsonization and phagocytosis.
- Disrupting quorum sensing: Interfering with quorum sensing can attenuate P. aeruginosa virulence and enhance the efficacy of antibiotics. Small molecules and enzymes that inhibit quorum sensing are under investigation as potential adjunct therapies.
Who is most at risk of contracting an infection from this bacteria
Pseudomonas aeruginosa primarily poses a threat to immunocompromised individuals and those with underlying medical conditions. The groups most at risk of contracting an infection from this bacterium include:
- Patients with cystic fibrosis: P. aeruginosa is a common cause of chronic lung infections in individuals with cystic fibrosis, leading to a decline in lung function over time.
- Hospitalized patients: P. aeruginosa is a leading cause of nosocomial (hospital-acquired) infections. Patients who undergo invasive medical procedures, have indwelling devices (e.g., urinary catheters, central venous catheters), or have undergone surgery are at increased risk.
- Immunocompromised individuals: People with weakened immune systems, such as those with HIV/AIDS, organ transplant recipients, or patients receiving chemotherapy or immunosuppressive medications, are more susceptible to P. aeruginosa infections.
- Burn patients: P. aeruginosa can cause severe skin and soft tissue infections in individuals with extensive burns, as their natural skin barrier is compromised.
- Patients with chronic wounds: Individuals with chronic, non-healing wounds, such as diabetic foot ulcers or pressure ulcers, are at increased risk for P. aeruginosa infections.
- Patients with chronic respiratory conditions: People with chronic obstructive pulmonary disease (COPD), bronchiectasis, or other chronic lung diseases are more susceptible to respiratory infections caused by P. aeruginosa.
Prevention and Control Measures
Preventing P. aeruginosa infections is essential, particularly in healthcare settings where vulnerable populations are at risk. Effective control measures include:
- Hand hygiene: Practicing proper hand hygiene among healthcare workers is crucial to prevent the spread of P. aeruginosa and other nosocomial pathogens.
- Environmental cleaning and disinfection: Regular cleaning and disinfection of surfaces, medical equipment, and high-touch areas can reduce the risk of P. aeruginosa transmission in healthcare facilities.
- Water system management: P. aeruginosa can thrive in water systems, including sinks, faucets, and showers. Regular monitoring and maintenance of water systems, including the use of disinfectants, can help minimize the risk of contamination.
- Device and catheter care: Proper insertion, maintenance, and removal of indwelling devices, such as urinary catheters and central venous catheters, are critical to preventing device-associated infections caused by P. aeruginosa.
- Antimicrobial stewardship: The judicious use of antibiotics is essential to slow down the emergence of antibiotic resistance. Implementing antimicrobial stewardship programs in healthcare facilities can promote appropriate antibiotic prescribing and optimize patient outcomes.